What’s the difference between a community health system and an academic medical center? To most, a hospital is simply a hospital. However, the rising pattern of university medical centers acquiring, merging, or partnering with community health systems calls for a closer look at the roles each plays in society.
Beyond the surface, what really separates community health systems from their academic counterparts? And what happens when the two come together? How does the integration of academic and community health systems affect each organization and, more importantly, their patients?
Academic medical centers versus community health systems
While both academic and community medical centers are dedicated to providing quality health care, their primary differences lie in their focus, culture, and services.
Academic medical centers (AMCs) are hubs of innovation and learning. Typically affiliated with medical schools and research institutions, they’re deeply involved in medical research, education, and training. At these centers, medical professionals work together to push the boundaries of medicine, with key characteristics of the institutions being:
- Research and education: AMCs prioritize medical research and education. These institutions are often where the latest medical breakthroughs are born and serve as training grounds for the next generation of healthcare professionals.
- Specialized care: Due to their focus on research and expertise, AMCs often offer specialized services and treatments for medical conditions. Patients may seek out AMCs for cutting-edge therapies and clinical trials.
- Complex cases: AMCs often handle complex medical cases as they tend to be equipped with state-of-the-art technology and specialists from various fields who can tackle challenging diagnoses and treatments.
On the other hand, community medical centers or health systems are deeply rooted in their communities, catering to the diverse needs of the local population. While community health systems may engage in research and education to some extent, their priority is to deliver comprehensive, accessible care to patients close to home.
Some key characteristics include:
- Primary and preventive care: Community health systems focus on addressing everyday healthcare needs through primary and preventive care. They deliver a broad spectrum of services tailored to the needs of their community, such as emergency care, maternity care, and routine screenings.
- Local engagement: Community health systems tend to build strong ties with local residents and healthcare providers. They may collaborate with local organizations and government agencies to address community health needs and promote health education initiatives.
- Accessibility: Community health systems prioritize accessibility and affordability, ensuring that essential healthcare services are available to all members of the community.
While both types of hospitals strive to provide excellent care, the differences in their cultures can have implications for patient experience and outcomes.
Academic medical centers may offer access to groundbreaking treatments and specialized expertise, which can result in better clinical outcomes for certain conditions. The atmosphere in these hospitals can be bustling and dynamic, with teams of specialists collaborating to tackle complex cases.
On the other hand, community health systems are typically much more accessible than AMCs, both in terms of convenient locations and lower costs, which can lead to greater patient satisfaction and adherence to treatment plans.
Why merge?
Recent years have seen a marked uptick in the merging of academic and community health systems. The trend of academic medical centers acquiring community hospital networks was noted in Kaufman Hall’s 2022 and 2023 merger and acquisition (M&A) reports, with the firm spotlighting a peak in Q3 2023, “when academic health systems acted as the acquirer in 50% of the fourteen transactions involving a not-for-profit acquirer.”
One of the biggest motives behind this trend appears to be the pursuit of financial stability. One analysis by the American Hospital Association and Kaufman Hall in 2021 suggested that nearly 40% of hospitals were financially challenged or distressed before an M&A transaction.
When academic medical centers and community health systems merge, they can use economies of scale, improve revenue streams, and enhance bargaining power with insurers and suppliers.
AMCs, while renowned for their research, teaching, and advanced medical care, increasingly face financial challenges due to their high-cost structures and reliance on government funding and research grants. On the other hand, community health systems, while essential for providing accessible care to local populations, may also struggle with limited resources and infrastructure.
When the two come together, they can experience cost savings through economies of scale, improved revenue streams, and enhanced bargaining power with insurers and suppliers. Additionally, AMCs can tap into the community health system’s patient base, expanding their reach and diversifying their revenue sources.
Proposed benefits for patients
While most mergers, acquisitions, and partnerships (MAP) in healthcare have historically been pursued for financial stability or greater competitiveness, the combined strength of academic and community health systems is also argued to (theoretically) provide plenty of benefits for patients. Some of these include:
Enhanced access to specialized care: By merging with community health systems, AMCs can extend their reach into local communities, bringing cutting-edge treatments and expertise closer to patients who may otherwise have limited access.
Improved quality of care: Potentially, the combined expertise, resources, and infrastructure can lead to enhanced clinical outcomes, reduced medical errors, and better coordination of care. Additionally, AMCs often bring quality improvement processes and protocols to the newly acquired or merged community hospital, which can positively impact patient safety and satisfaction.
Economies of scale: Combining resources could also lead to cost efficiencies, allowing for better allocation of funds toward patient care, infrastructure improvement, and technology upgrades. This would lower the overall cost of healthcare delivery, benefiting both patients and the healthcare system.
Increased research opportunities: By partnering with community health systems, AMCs can leverage a larger patient population for clinical trials and research studies, accelerating the pace of medical advancements.
Stronger bargaining power: With a larger patient base, the merged entity enhances its leverage with insurers and suppliers. This can lead to more favorable reimbursement rates and access to essential medical supplies, ultimately benefiting patients by improving the affordability of care.
While these theoretical benefits hold promise, they are far from guaranteed, with there being much debate on whether the integration of the two health systems can consistently produce the above outcomes.
Expectations versus reality
As with any initiative, the reality is more nuanced. While there are success stories where MAP activities have revitalized struggling hospitals and enhanced patient care, there are also instances where the effort failed to live up to expectations.
The good news? Patients at community hospitals acquired by academic medical centers do often gain improved access to more specialized services. M&As have also been effective at keeping many financially struggling hospitals open, ensuring local communities keep that access to care.
However, research indicates a mixed bag when it comes to quality of care. While quality improvement initiatives and protocol standardization regularly occur, the overall impact on care quality varies.
On one hand, a study by JAMA Network Open showed rural hospital mergers reduced mortality rates for conditions like heart attacks, heart failure, strokes, and pneumonia, with the authors concluding that “these findings suggest that rural hospital mergers were associated with quality improvement.”
Patients at community hospitals acquired by academic medical centers do often gain improved access to more specialized services but it’s unclear if care quality improves.
At the University of Colorado Denver, a joint venture between academic and community hospitals has successfully led to the sharing of “data, expertise, and important quality and safety measures,” uplifting all parties involved.
On the other hand, a systematic review of the impact of hospital mergers found “no strong evidence of improvement or worsening healthcare quality measures.” Even more, a study of hospital mergers and acquisitions from 2009 to 2013 observed “modest deterioration in patient experiences,” along with “small and nonsignificant changes in readmission and mortality rates and inconclusive effects on performance on clinical-process measures.”
Whether MAP activity reduces costs for patients is also up for debate. One Charles River report revealed a 3.7% drop in revenue per admission at acquired hospitals compared to non-merging ones, suggesting that cost savings are transferred to patients and health plans. On the flip side, according to the Michigan Journal of Medicine, prices tend to rise when providers consolidate, indicating that anticipated cost efficiencies didn’t materialize or weren’t passed on to consumers.
Evidently, while the merging of community health systems with academic medical centers holds promise, it’s also a complex undertaking with no guaranteed outcomes. So what does it take for these different entities to successfully integrate and thrive together?
Getting it right: why alignment matters
Successful collaborations between community and academic medical centers hinge on more than just combining expertise and resources — they demand quantifiable goals for improvement and proactive implementation strategies.
As McKinsey & Company puts it, partnerships must define specific sources of value from the beginning. Expectations that are too vague or ambitious can quickly lead to disappointment. The two parties must be aligned on the expected value for patients and themselves, as well as each other’s role in creating that value.
McKinsey suggests starting with a simple set of value drivers before gradually expanding goals over time. Focusing on achievable objectives within a manageable time frame allows for small, early wins that prove the partnerships’ value and pave the way for continued growth and collaboration.
In essence, the establishment of new goals and values serves as the foundation of the merged entity’s identity — its new brand promise. However, to truly deliver on this promise, it’s essential to ensure that organizational alignment extends both internally and externally.
The establishment of new goals and values serves as the foundation of the merged entity’s identity — its new brand promise.
Internally, this may require mapping stakeholder relationships, addressing cultural disparities, and aligning values, behaviors, and decision-making processes. Employees need to understand the rationale and goals behind the integration and how it benefits both systems. When every member is informed, the result is a unified and purpose-driven entity.
Externally, alignment involves ensuring that the brand promise resonates with patients, partners, and the broader community. Consistency in messaging and actions across all touchpoints reinforces trust and confidence in the merged entity’s ability to deliver on its commitments. This approach enhances cohesion between the integrating parties, strengthening their ability to deliver on their new, joint brand promise.
Ultimately, the success of mergers and acquisitions between community and academic medical centers hinges on purposeful action guided by clear objectives, effective communication, and strategic alignment of values and goals. Only by proactively embracing these principles can healthcare institutions realize their vision of ensuring the best possible outcomes for their patients, employees, and communities.
If you’re interested in exploring how Tronvig can assist your organization in achieving strategic alignment and advancing your healthcare marketing initiatives, contact us to learn more about our services.
*AI statement: I, Therese Nguyen, attest that I am the author of this article, but I generated an outline of the content using ChatGPT 4. I then wrote and edited the post in order to align the article with the standards for this blog.
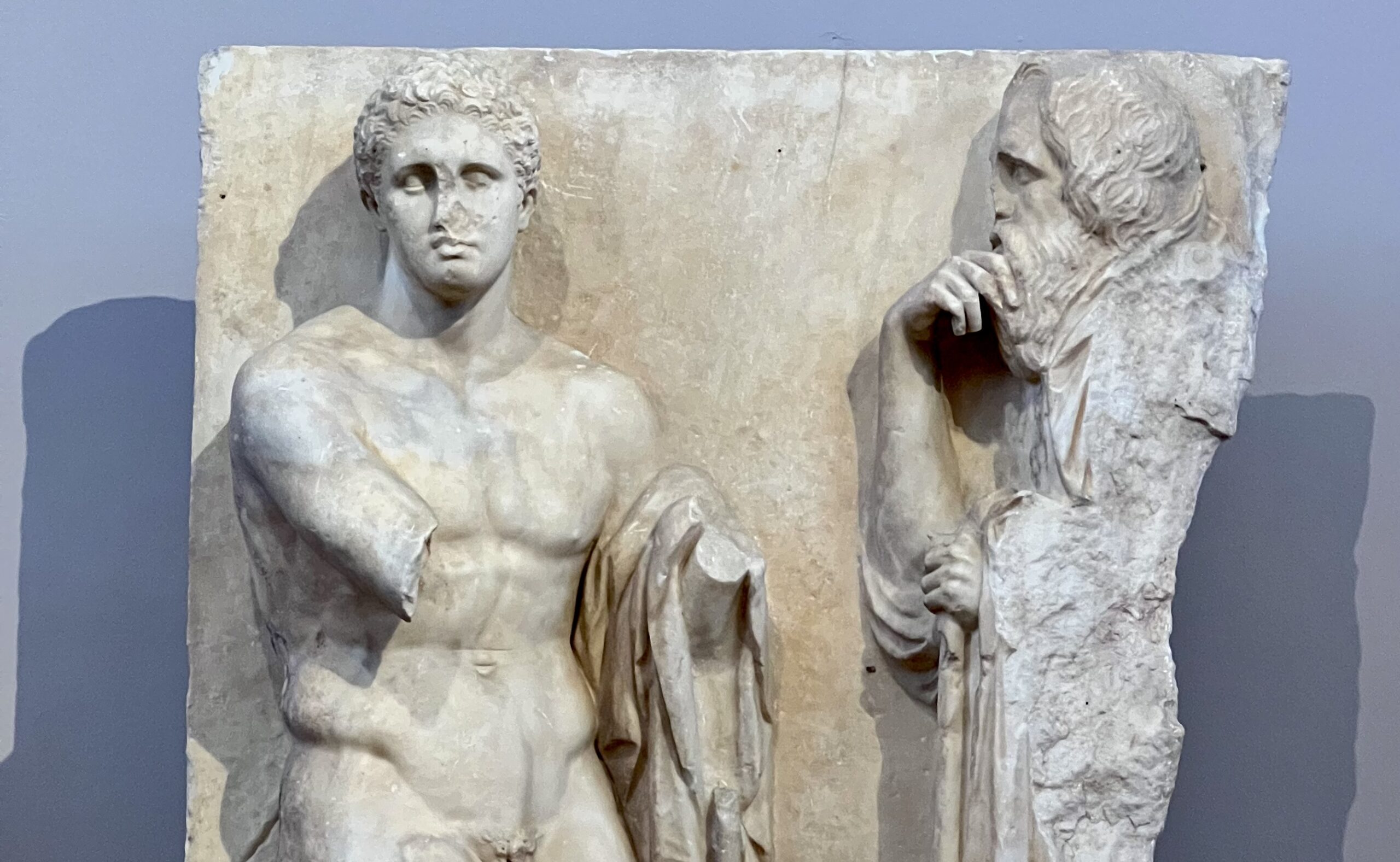
Photo by James Heaton at the National Archeological Museum in Athens

Ask for help.
We are kind, thorough and ready when you are. You just need to ask.