Healthcare is a deeply personal issue that impacts all of us. And yet, it’s also incredibly complicated, with many of us struggling to fully understand how our healthcare system works.
Whether choosing a doctor, figuring out insurance options, or simply trying to afford care or a hospital visit, navigating the healthcare world can often be frustrating and overwhelming. This complexity leads many to question the broader systems in place.
 In an era of constant debate about the “best” healthcare system, learning about different models is crucial. From free market principles to monopolistic practices, how do these approaches impact things like affordability, innovation, patient choice, and health outcomes? By understanding how these economic models shape our health services, we can better follow policy discussions and changes and make informed decisions for the future.
In an era of constant debate about the “best” healthcare system, learning about different models is crucial. From free market principles to monopolistic practices, how do these approaches impact things like affordability, innovation, patient choice, and health outcomes? By understanding how these economic models shape our health services, we can better follow policy discussions and changes and make informed decisions for the future.
The free market in healthcare
Let’s first dive into what it would look like if true free market principles were applied in the health space.
In its purest form, the free market is a system in which goods and services are exchanged voluntarily between parties without government intervention. This model is rooted in principles of supply and demand, with prices being determined by the balance between what consumers are willing to pay and what producers are willing to offer.
Theoretically, applying free market principles to healthcare could offer (though, not guarantee) several benefits. Increased competition among providers can drive down prices, encourage innovation, and ultimately lead to improved quality of services as providers compete to attract more patients.
Healthcare is not like any other traditional good or service so the way the healthcare market operates deviates from traditional market dynamics.
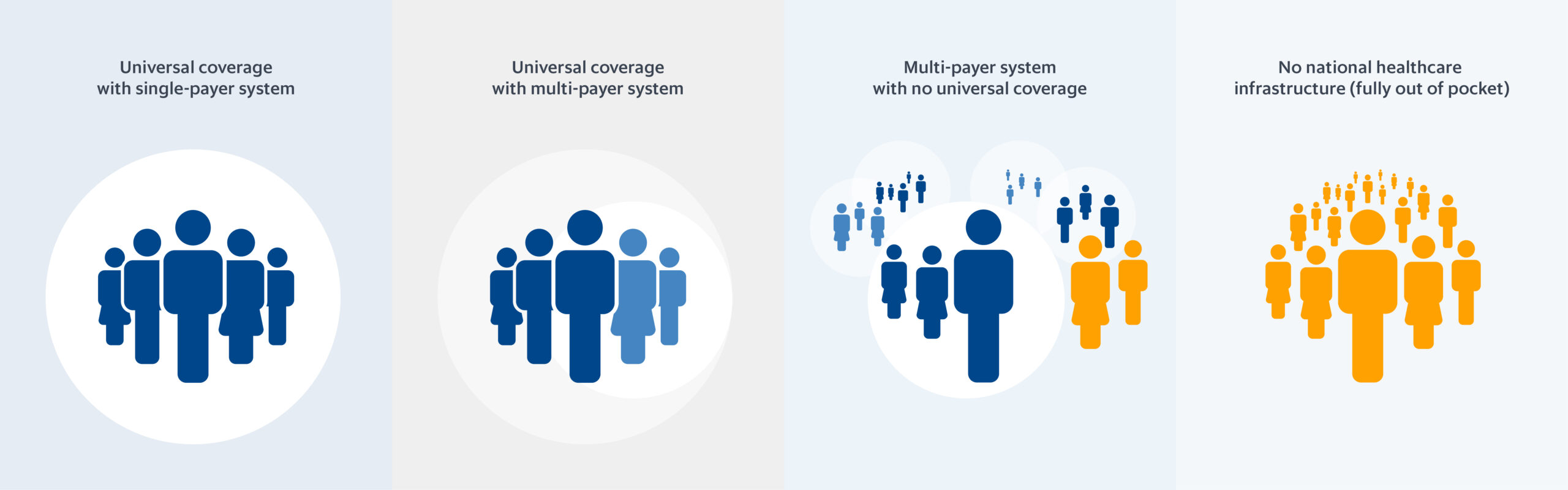
Called the Uninsured or Out-Of-Pocket Model, “free-market” healthcare systems do exist, though mostly in low-income countries that don’t have the resources to fund a robust healthcare system. In these cases, you, as the consumer, would pay hospitals and healthcare providers directly and out-of-pocket, much like any other commodity.
However, healthcare is not like any other traditional good or service. This means the way the healthcare market operates actually deviates from traditional market dynamics.
How the healthcare market differs
Firstly, there’s significant information asymmetry between patients and providers. Unlike purchasing a car or a smartphone, patients typically lack the expertise to fully evaluate medical treatments or procedures, placing them at a disadvantage in negotiating prices.
Healthcare demand is also largely inelastic. In other words, demand remains relatively unchanged even when prices go up or down. After all, when faced with illness or injury, most people will seek doctors and medical care regardless of cost. This could lead to limited price sensitivity and exploitative pricing practices (rather than competitive pricing argued under free market theories).
Healthcare generates positive externalities, meaning that individual health outcomes can benefit society as a whole.
Finally, healthcare generates positive externalities, meaning that individual health outcomes can benefit society as a whole. Because the social value of healthcare extends beyond the immediate transaction between patient and provider, having the value of healthcare determined by supply and demand gets complicated since patients seldom consider the true societal value of health services (think: vaccines).
These complexities are why government regulations and insurance companies have such a presence in the industry. Regulation aims to ensure patient safety, enforce fair market practices, and promote public health. Meanwhile, insurance mitigates the financial risks associated with unpredictable healthcare expenses.
When government and insurance join the mix
When government and insurance companies become part of the healthcare equation, three overarching models often emerge, though many countries implement a combination or modified version of these models.
The Bismarck model
The Bismarck Model, originating in Germany, features a multi-payer insurance system funded by employers and employees through payroll deductions. While the insurance companies and healthcare providers are typically private, insurance plans are non-profit and must cover everyone, with the government regulating costs and requiring universal coverage.
Advantages:
- Universal coverage. By making health insurance compulsory, the Bismarck model aims to provide healthcare coverage to all citizens, ensuring that everyone has access to necessary medical services.
- Choice of providers. Individuals can choose their insurance and healthcare providers, which provides patients with a degree of autonomy and flexibility in their healthcare decisions.
- Cost sharing. Costs are split between employers and employees, which spreads the financial cost of healthcare across the workforce and alleviates the burden on individuals.
- Market competition. This model encourages competition among various health insurance funds and healthcare providers, which can lead to innovation, efficiency, and higher quality of care as organizations strive to attract members and improve services.
Disadvantages:
- Administrative complexity. Dealing with multiple insurance companies, each with its own rules, coverage options, and reimbursement procedures, can lead to inefficiencies caused by administrative complexity and paperwork burdens.
- Higher costs. Administrative costs can be high due to multiple insurance companies and complex billing processes. Balancing cost control while maintaining competition can also be difficult.
- Inequitable access and fragmented coverage. Despite its aim of universal coverage, this model may still result in inequitable access to healthcare. Factors like socioeconomic status, employment status, and geographic location influence whether you can easily access insurance or afford greater coverage.
- Monopoly risks. Over time, there may be a risk of monopolies and oligarchies, where a few large insurers or healthcare providers dominate the market, potentially stifling competition and driving up costs.
The Beveridge model
Often referred to as a single-payer system, the Beveridge Model was developed in the United Kingdom. In this model, healthcare is directly provided and financed by the government through tax payments. Many hospitals and clinics are government-owned, and healthcare providers are government employees.
Advantages:
- Universal coverage. Healthcare is provided to all citizens regardless of their ability to pay, ensuring that everyone has access to essential healthcare services.
- Equity. Under this model, healthcare access is based on need rather than ability to pay. This helps reduce disparities in healthcare access and outcomes among different socioeconomic groups.
- Cost efficiency. By operating as a single-payer system, this model could reduce administrative costs associated with managing multiple insurance plans. This can lead to cost savings and more efficient use of healthcare resources.
- Preventive care emphasis. Intending to promote public health, Beveridge systems often emphasize preventative care and early intervention, potentially reducing the burden of expensive treatments for preventable diseases later on.
Disadvantages:
- Funding challenges. Relying on taxes can be politically and economically challenging, as well as a burden for taxpayers, especially in times of economic downturn or an aging population. Plus, government budget constraints can impact the availability and quality of services.
- Long wait times. The demand for healthcare services may surpass the available resources of the public healthcare system, leading to long wait times for certain procedures or treatments.
- Limited choice. Patients may have limited options in terms of healthcare providers and treatments since services are often provided by government-run institutions.
- Inefficiencies and innovation constraints. Government control may lead to bureaucratic inefficiencies while also stifling innovation in medical technologies and treatments due to centralized decision-making and reduced incentives for private investment.
The National Health Insurance model
The National Health Insurance model blends elements of the Beveridge and Bismarck systems. It features a single-payer, government-run insurance program funded by taxes, but healthcare services are delivered by private providers.
Advantages:
- Universal coverage. Everyone is covered under the national insurance plan.
- Equitable access. By removing financial barriers to healthcare, such as co-pays and deductibles, this model promotes equitable access to necessary medical services.
- Simplified administration. A single-payer system can simplify administrative processes and costs for both patients and healthcare providers by reducing paperwork, billing complexities, and the need to navigate multiple insurance plans.
- Cost efficiency. By pooling resources and spreading risk across the entire population, this model can potentially reduce administrative costs and achieve lower prices for medical services and medications.
Disadvantages:
- Funding challenges. Funding the system through taxes can be challenging, as government funding can be unpredictable and impacted by changes in political priorities, economic downturns, and an aging population.
- Inefficiencies. Government-run insurance can become bogged down with bureaucracy, leading to inefficiencies that lead to mismanagement or slower response to healthcare needs.
- Long wait times. Similar to the Beveridge model, the universal nature of the system can result in longer wait times for certain services when demand surpasses supply.
- Limited choice. Those covered under the NHI may have limitations on the choice of healthcare providers or delays in accessing certain services, leading to concerns about freedom of choice and quality of care for patients.
The U.S. healthcare system: a complicated combination
Unlike many other countries, the United States has “no single nationwide system of health insurance.” Instead, it’s a combination of various models and approaches resulting in a complex and often confusing landscape.
Elements of all four major healthcare models (the three described in the previous section plus the Uninsured model) can be found within the U.S. healthcare system.
At its core, the U.S. healthcare system is predominantly driven by private insurance, with about 65.6% of the population covered by private plans in 2022. This mirrors aspects of the Bismarck model, especially in how multiple private insurance companies and healthcare providers compete for consumers.
In a way, the Affordable Care Act attempted to bring the U.S. system closer to the universal coverage aspect of the Bismarck model, with regulations that mandated insurance coverage, strengthened consumer protections, and provided subsidies for private insurance. While the ACA did increase coverage, it also faced political opposition and legal challenges, with the health insurance mandate repealed in 2017.
The Department of Veterans Affairs (VA), the Indian Health Service, and the Federal Bureau of Prisons operate under the Beveridge model. Under these agencies, the government owns the facilities and employs healthcare professionals.
Medicare and Medicaid resemble the National Health Insurance model. These public health insurance programs are funded by the government but use private providers to deliver healthcare services. Medicare serves primarily older adults while Medicaid assists low-income individuals and families.
Finally, as of late 2023, around 7.7% of the population experience the Uninsured model. More than 25 million Americans lack health insurance and pay out-of-pocket for medical services. While emergency rooms are required to provide care regardless of ability to pay, this does not extend to other healthcare services, leaving many without necessary care.
Why this all matters
The complex nature of the U.S. healthcare system underscores the ongoing discussion over how best to provide and finance healthcare for its citizens. As policymakers and stakeholders continue to debate and shape the future of healthcare, understanding the foundational models is essential.
Studying these approaches means we take an important step toward knowing how our healthcare system operates. By recognizing the different models and their implementations within the U.S., we can better assess the strengths and weaknesses that exist in the current structure.
Of course, this discussion only scratches the surface of a multifaceted topic. While we’ve touched on key points, there’s much more to learn and understand. Getting informed about the dynamics at play empowers us to make educated decisions about our healthcare and engage meaningfully in discussions about its future. In doing so, we can better comprehend the complexities and advocate for a healthcare system that serves us all.
*AI statement: I, Therese Nguyen, attest that I am the author of this article, but I generated an outline of the content using ChatGPT 4. I then wrote and edited the post in order to align the article with the standards for this blog.
Photo courtesy of iStock

Ask for help.
We are kind, thorough and ready when you are. You just need to ask.